I-pneumonia etholwe ngumphakathi kubantu abadala

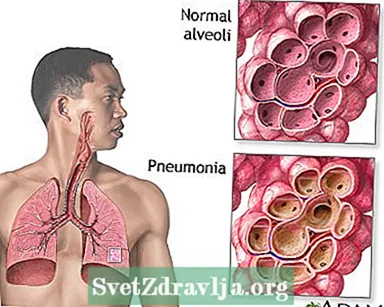
I-pneumonia yisimo sokuphefumula (sokuphefumula) lapho kukhona ukutheleleka kwamaphaphu.
Lo mbhalo uhlanganisa inyumoniya etholwe ngumphakathi (i-CAP). Lolu hlobo lwe-pneumonia lutholakala kubantu abangakafiki esibhedlela noma kwenye indawo yokunakekelwa kwezempilo efana nekhaya labahlengikazi noma indawo yokuvuselela. I-pneumonia ethinta abantu abasezikhungweni zokunakekelwa kwezempilo, njengezibhedlela, ibizwa ngokuthi inyumoniya etholakala esibhedlela (noma inyumoniya ehlobene nokunakekelwa kwezempilo).
I-pneumonia yisifo esivamile esihlasela izigidi zabantu unyaka nonyaka e-United States. Amagciwane abizwa ngamagciwane, amagciwane nesikhunta angadala inyumoniya. Kubantu abadala, amagciwane ayimbangela ejwayelekile kakhulu ye-pneumonia.
Izindlela ongathola ngazo inyumoniya zifaka:
- Amagciwane namagciwane ahlala emakhaleni akho, amasinusi, noma umlomo ungasakazekela emaphashini akho.
- Ungaphefumulela amanye ala magciwane ngqo emaphashini akho.
- Uphefumula (udonsa) ukudla, iziphuzo, uhlanza, noma uketshezi oluvela emlonyeni uye emaphashini akho (i-aspiration pneumonia).

I-pneumonia ingadalwa yizinhlobo eziningi zamagciwane.
- Uhlobo oluvame kakhulu lwama-bacteria yi- I-Streptococcus pneumoniae (i-pneumococcus).
- I-pneumonia engavamile, evame ukubizwa ngokuthi i-pneumonia yokuhamba, ibangelwa amanye amabhaktheriya.
- Isikhunta esibizwa I-Pneumocystis jiroveci kungadala inyumoniya kubantu amasosha omzimba wabo angasebenzi kahle, ikakhulukazi abantu abanesifo se-HIV esithuthukile.
- Amagciwane, njengegciwane lomkhuhlane, futhi muva nje i-SARS-CoV-2 (edala i-COVID-19), nazo ziyizimbangela ezivamile zenyumoniya.
Izici zobungozi ezandisa amathuba akho okuthola i-pneumonia zifaka:
- Isifo samaphaphu esingamahlalakhona (COPD, bronchiectasis, cystic fibrosis)
- Ukubhema ugwayi
- Ukuwohloka komqondo, isifo sohlangothi, ukulimala ebuchosheni, ukukhubazeka kobuchopho, noma okunye ukuphazamiseka kobuchopho
- Inkinga yesistimu yomzimba (ngesikhathi sokwelashwa komdlavuza, noma ngenxa ye-HIV / AIDS, ukufakelwa komzimba, noma ezinye izifo)
- Ezinye izifo ezibucayi, njengesifo senhliziyo, isifo sokuqina kwesibindi noma isifo sikashukela
- Ukuhlinzwa kwakamuva noma ukuhlukumezeka
- Ukuhlinzwa ukwelapha umdlavuza womlomo, womphimbo, noma wentamo
Izimpawu ezivame kakhulu ze-pneumonia yilezi:
- Ukukhwehlela (ngezinye izifo zamaphaphu ungakhwehlela isikhwehlela esiluhlaza noma esiphuzi, noma umchamo onegazi)
- Imfiva, engahle ibe mncane noma iphezulu
- Ukunyakazisa amakhaza
- Ukuphefumula (kungenzeka kuphela uma ukhuphuka izitebhisi noma uzikhandla)
Ezinye izimpawu zifaka:
- Ukudideka, ikakhulukazi kubantu abadala
- Ukujuluka okweqile nesikhumba se-clammy
- Ubuhlungu bekhanda
- Ukuphelelwa isifiso sokudla, amandla amancane, nokukhathala
- UMalaise (akazizwa kahle)
- Ubuhlungu besifuba obucijile noma obugwinyayo obuba nzima lapho uphefumula kakhulu noma ukhwehlela
- I-White nail syndrome, noma i-leukonychia

Umhlinzeki wezokunakekelwa kwempilo uzolalela imfantu noma imisindo yokuphefumula engajwayelekile lapho elalela isifuba sakho nge-stethoscope. Ukushaya odongeni lwesifuba sakho (ukushayisana) kusiza umhlinzeki alalele futhi azizwe ngemisindo engajwayelekile esifubeni sakho.
Uma kusolwa i-pneumonia, umhlinzeki uzo-oda i-x-ray yesifuba.
Ezinye izivivinyo ezinga-odwa zifaka:
- Imithambo yegazi yegazi ukubona ukuthi umoya-mpilo owanele ungena yini egazini lakho kusuka emaphashini.
- Amasiko egazi nesikhwehlela ukubheka igciwane elingahle lidale inyumoniya.
- I-CBC ukuhlola isibalo samaseli amhlophe egazi.
- I-CT scan yesifuba.
- I-Bronchoscopy. Ishubhu eliguquguqukayo elinekhamera ekhanyisiwe ekugcineni idluliselwe emaphashini akho, ezimweni ezikhethiwe.
- Thoracentesis. Ukususa uketshezi esikhaleni esiphakathi kolwelwesi lwangaphandle lwamaphaphu nodonga lwesifuba.
- I-Nasopharyngeal swab ukuhlola amagciwane afana nomkhuhlane kanye ne-SARS-CoV-2.
Umhlinzeki wakho kufanele aqale anqume ukuthi udinga yini ukuba sesibhedlela. Uma welashwa esibhedlela, uzothola:
- Uketshezi namagciwane ngemithambo yakho
- Ukwelashwa kwe-oxygen
- Imishanguzo yokuphefumula (mhlawumbe)
Uma kutholakala ukuthi unohlobo lwe-pneumonia olunegciwane, kubalulekile ukuthi uqalwe kuma-antibiotic ngokushesha okukhulu ngemuva kokungeniswa. Uma une-pneumonia yegciwane, ngeke uthole ama-antibiotic. Lokhu kungenxa yokuthi ama-antibiotics awabulali amagciwane. Ungathola eminye imithi, njengemithi elwa namagciwane, uma uphethwe umkhuhlane.
Kungenzeka ukuthi ungeniswe esibhedlela uma:
- Unenye inkinga enkulu yezokwelapha
- Yiba nezimpawu ezinzima
- Awukwazi ukuzinakekela ekhaya, noma awukwazi ukudla noma ukuphuza
- Badala kunama-65
- Bengilokhu ngithatha ama-antibiotics ekhaya futhi angabi ngcono
Abantu abaningi bangelashwa emakhaya. Uma kunjalo, umhlinzeki wakho angakutshela ukuthi uthathe imithi efana nama-antibiotic.
Lapho uthatha ama-antibiotic:
- Ungaphuthelwa noma yimiphi imithamo. Thatha umuthi uze uphele, noma ngabe uqala ukuzizwa ungcono.
- Ungathathi umuthi wokukhwehlela noma umuthi obandayo ngaphandle kokuthi udokotela wakho athi kulungile. Ukukhwehlela kusiza umzimba wakho ukukhipha amafinyila emaphashini akho.
Ukuphefumula umoya oshisayo, omanzi (omanzi) kusiza ukukhulula amafinyila anamathele angakwenza uzizwe sengathi uyakhinka. Lezi zinto zingasiza:
- Beka indwangu yokufudumala emanzi ngokukhululekile phezu kwekhala lakho nomlomo.
- Gcwalisa umswakama ngamanzi afudumele bese uphefumulela enkungwini efudumele.
- Thatha ukuphefumula okumbalwa izikhathi ezi-2 noma ezi-3 njalo ngehora. Ukuphefumula okujulile kuzosiza ukuvula amaphaphu akho.
- Thepha isifuba sakho kamnandi izikhathi ezimbalwa ngosuku ngenkathi ulele ikhanda lakho liphansi kunesifuba sakho. Lokhu kusiza ukukhuphula amafinyila emaphashini ukuze ukwazi ukukhwehlela.
Phuza iziphuzo eziningi, inqobo nje uma umhlinzeki wakho ethi kulungile.
- Phuza amanzi, ujusi, noma itiye elibuthakathaka
- Phuza okungenani izinkomishi eziyi-6 kuye kwezingu-10 (1.5 kuya ku-2.5 litre) ngosuku
- Ungaphuzi utshwala
Thola ukuphumula okuningi lapho uya ekhaya. Uma unenkinga yokulala ebusuku, phumula kancane emini.
Ngokwelashwa, abantu abaningi bayathuthuka kungakapheli amasonto ama-2. Abantu abadala asebekhulile noma abantu abagula kakhulu bangadinga ukwelashwa okude.
Labo abangase babe namathuba amaningi okuba nenyumoniya eyinkimbinkimbi bahlanganisa:
- Abantu abadala asebekhulile
- Abantu amasosha omzimba wabo angasebenzi kahle
- Abantu abanezinye izinkinga ezinkulu zezokwelapha ezifana nesifo sikashukela noma i-cirrhosis yesibindi
Kuzo zonke lezi zimo ezingenhla, inyumoniya ingaholela ekufeni, uma inzima.
Ezimweni ezingavamile, izinkinga ezinkulu kakhulu zingakhula, kufaka phakathi:
- Izinguquko ezisongela impilo emaphashini ezidinga umshini wokuphefumula
- Uketshezi oluzungeze iphaphu (pleural effusion)
- Uketshezi oluthelelekile oluzungeze iphaphu (empyema)
- Amathumba emaphaphu
Umhlinzeki wakho anga-oda enye i-x-ray. Lokhu kwenzelwa ukuthi amaphaphu akho acace. Kepha kungathatha amasonto amaningi ukuthi i-x-ray yakho icace. Ungahle uzizwe ungcono ngaphambi kokuthi i-x-ray isule.
Shayela umhlinzeki wakho uma une:
- Ukukhwehlela okuletha amafinyila anegazi noma ukugqwala
- Izimpawu zokuphefumula (zokuphefumula) eziba zimbi kakhulu
- Ubuhlungu besifuba buba bubi kakhulu uma ukhwehlela noma uphefumulela ngaphakathi
- Ukuphefumula okusheshayo noma okubuhlungu
- Ukujuluka ebusuku noma ukuncipha kwesisindo okungaqondakali
- Ukuphefumula okuncane, ukuqhaqhazela okubandayo, noma imfiva ephikelelayo
- Izimpawu zenyumoniya namasosha omzimba abuthakathaka (ngokwesibonelo, njenge-HIV noma i-chemotherapy)
- Ukuqina kwezimpawu ngemuva kokuthuthuka kokuqala
Ungasiza ukuvimbela inyumoniya ngokulandela izinyathelo ezingezansi.
Geza izandla zakho kaningi, ikakhulukazi:
- Ngaphambi kokulungiselela nokudla ukudla
- Ngemuva kokushaya amakhala
- Ngemuva kokuyogeza
- Ngemuva kokushintsha inabukeni lengane
- Ngemuva kokuhlangana nabantu abagulayo
Gwema ukuthintana nabantu abagulayo.
Ungabhemi. Ugwayi ulimaza ikhono lamaphaphu akho lokulwa nokutheleleka.
Imithi yokugoma ingasiza ekuvikeleni ezinye izinhlobo zenyumoniya. Qiniseka ukuthi uthola imigomo elandelayo:
- Umuthi wokugomela umkhuhlane ungasiza ekuvikeleni inyumoniya ebangelwa igciwane lomkhuhlane.
- Umuthi wokugoma we-pneumococcal wehlisa amathuba akho okuthola inyumoniya kusuka I-Streptococcus pneumoniae.
Imithi yokugoma ibaluleke kakhulu kubantu abadala asebekhulile kanye nabantu abanesifo sikashukela, i-asthma, i-emphysema, i-HIV, umdlavuza, abantu abafakelwa izitho zomzimba, noma ezinye izimo zesikhathi eside.
I-bronchopneumonia; I-pneumonia etholwe ngumphakathi; I-CAP
- I-bronchiolitis - ukukhipha
- Imikhuhlane nomkhuhlane - yini ongayibuza udokotela wakho - umuntu omdala
- Imikhuhlane nomkhuhlane - yini ongayibuza udokotela - ingane yakho
- Ungaphefumula kanjani uma ushoda ngokuphefumula
- Ukuphepha kwe-oksijeni
- I-pneumonia kubantu abadala - ukukhipha
- I-pneumonia ezinganeni - ukukhipha
- Usebenzisa i-oxygen ekhaya
- Usebenzisa i-oxygen ekhaya - ukuthi ubuze ini kudokotela wakho
- Lapho ingane noma usana lwakho lunomkhuhlane
 Uhlelo lokuphefumula
Uhlelo lokuphefumula Inyumoniya
Inyumoniya I-White nail syndrome
I-White nail syndrome
UDaly JS, u-Ellison RT. I-pneumonia enamandla. Ku: Bennett JE, Dolin R, Blaser MJ, ama-eds. Mandell, Douglas, kanye neBennett's Principles and Practice of Infectious Diseases. Umhlaka 9. IPhiladelphia, PA: Elsevier; 2020: isahluko 67.
UMusher DM. Sibutsetelo se-pneumonia. Ku: IGoldman L, iSchafer AI, ama-eds. Imithi yeGoldman-Cecil. Umhla ka-26. IPhiladelphia, PA: Elsevier; 2020: isahluko 91.
I-Wunderunk RG. Imihlahlandlela yokuphatha inyumoniya etholwe ngumphakathi. Umtholampilo Chest Med. 2018; 39 (4): 723-731. I-PMID: 30390744 pubmed.ncbi.nlm.nih.gov/30390744/.
